Best Practices for Successful EHR Data Integration
Best Practices for Successful EHR Data Integration
Electronic Health Records or EHRs are widely used nowadays as almost all hospitals use a certified EHR system. But even today, successful EHR integration remains an issue for many. For instance, in 2015, 3 out of 5 hospitals could not successfully integrate their data into the EHRs. This results in efficiency-related issues, making operating costs unnecessarily higher.
Why is EHR integration so crucial?
In the current model of data-driven healthcare in the country, EHR integration ensures that a hospital and the patient gets the maximum out of the available resources. There are numerous EHR systems and software available today. With new regulations that promote the adoption of EHRs as well as the development of applications, wearable technologies, and the Internet of Things, having a common pool of data is extremely beneficial in delivering the best healthcare treatments.
Unlike standard commerce and retail establishments, where companies could be using three or four different kinds of systems, healthcare organizations could be using anywhere up to 500 different systems and software. It becomes difficult to communicate across different systems, and that reduces the efficacy of the whole system that has been put in place. It’s crucial that all the entities try to connect all these dots to synchronize the information for everyone’s benefit.
Why is EHR integration an issue?
Even when healthcare providers understand the problems of setting up two systems working side by side, it remains a challenge to make these two systems communicate with each other. Here are some issues faced in EHR integration:
- Compatibility
There are thousands of EHRs systems out there, each with a unique schema, system architecture, service model, and strengths. This makes remote data extraction and sharing out of EHR difficult. - Methodology
Two different EHR systems have two different documentation practices that vary from one provider to another. This makes a successful interpretation of data by the other party challenging. - Conversion of data
Data received during the integration of EHR can be in different formats. Recording, formatting, and standardizing the data is needed to save all the critical info in a standard format. However, in this process, it’s critical to ensure that the essential meaning of the data is protected. - Transfer of data
Transferring data in packets from or to EHRs is a complex task and involves prior planning to ensure the safety of data. There are four major issues with data migration:- Network restrictions
- Hardware restrictions
- Unavailability of data during migration
- Risk of data loss in migration state
EHR integration solutions
Many players in recent times have tried to make this process smoother. Several EHR developers have created open APIs for operators to simplify the integration of data with their EHRs.
The good thing is that the will of healthcare providers to share healthcare data among each other is commendable. Data pools and the analytical tools available provide the necessary actionable intelligence required to maximize the potential of EHRs.
Some vendors use a big data-based data pool that enables healthcare providers to streamline the process of extract, transform, and load (ETL). Developing such an integrated data management platform is crucial when shifting to value-based care.
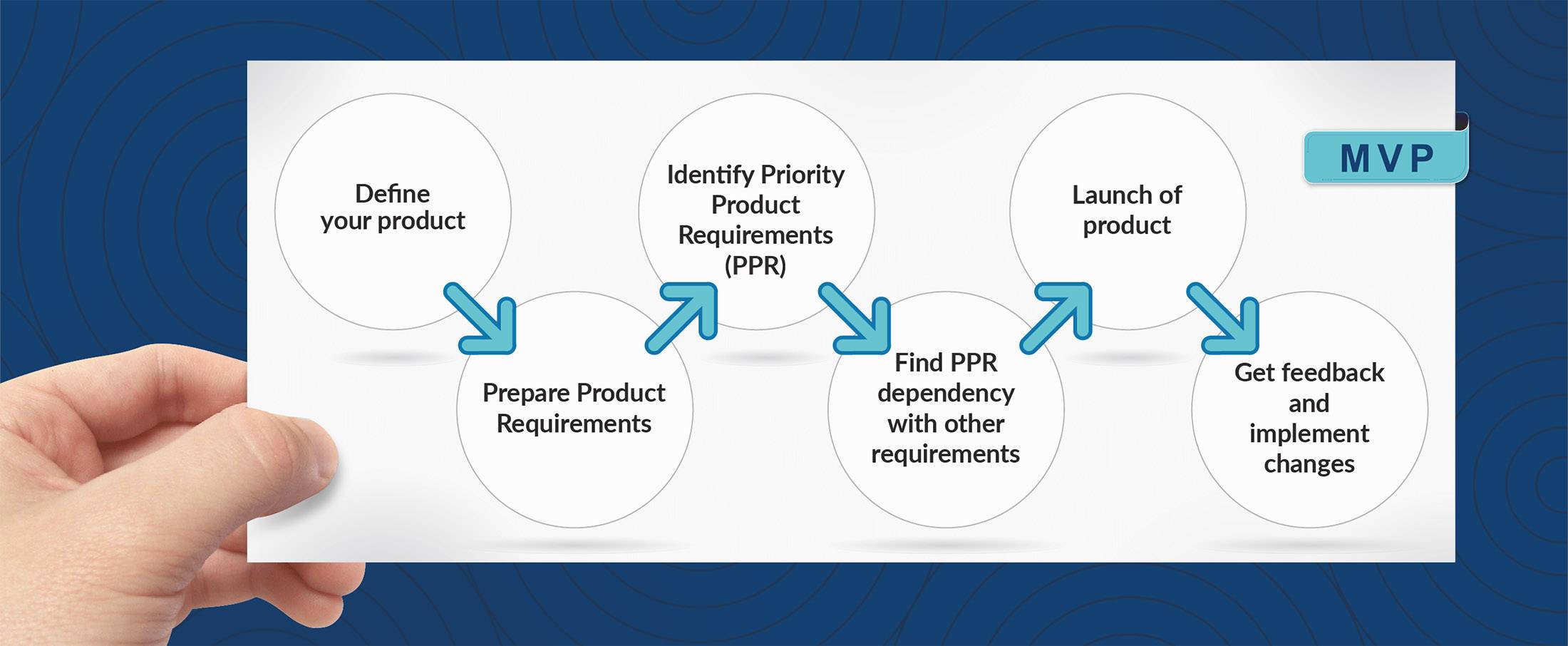
A strategy
There are many data management systems marketed to healthcare organizations, each with their own benefits and challenges. Given the rate of transformation in the healthcare sector, being dynamic and agile is crucial for success.
There is a need for step-by-step integration to tackle the challenges posed by lack of EHR Data Integration, such as: –
- Data Acquisition
The data pool must have pre-built connectors to many other EHR systems. The data pool must be able to extract data from every EHR, regardless of whether the other EHR has an API or standard architecture. - Data Cleaning
The data pool must work on detecting duplicate records, incomplete entries, improperly formatted, or data that has become old. It must find if the data went through bad parsing of record fields. - Data Compatibility
All the data imported must be standardized with advanced tools to bring all the necessary information in the patient care process, in a single format. - Data Quality
Agile algorithms must be employed to identify bad values, missing data, non-standard values formats, and must be able to perform a complete audit of the data imported to ensure there are no broken transformations. It should be able to take corrective measures to improve data quality.
- Big Data
- EHR Integration
- ETL
- Extract-Transform-Load
- Healthcare
Mobifilia
13 April 2020